Publish Tuesday evening
tl;dr – I got a CT scan at Big Cancer Center, and it was a lot more of a nuisance than prior scans. I can only hope it’s worth it.
Background
I set aside this full week for visiting Big Cancer Center to get a second opinion on treatment for my recurrence. I already met my assigned oncologist on Monday and went to get some bloodwork, which was amazingly efficient.
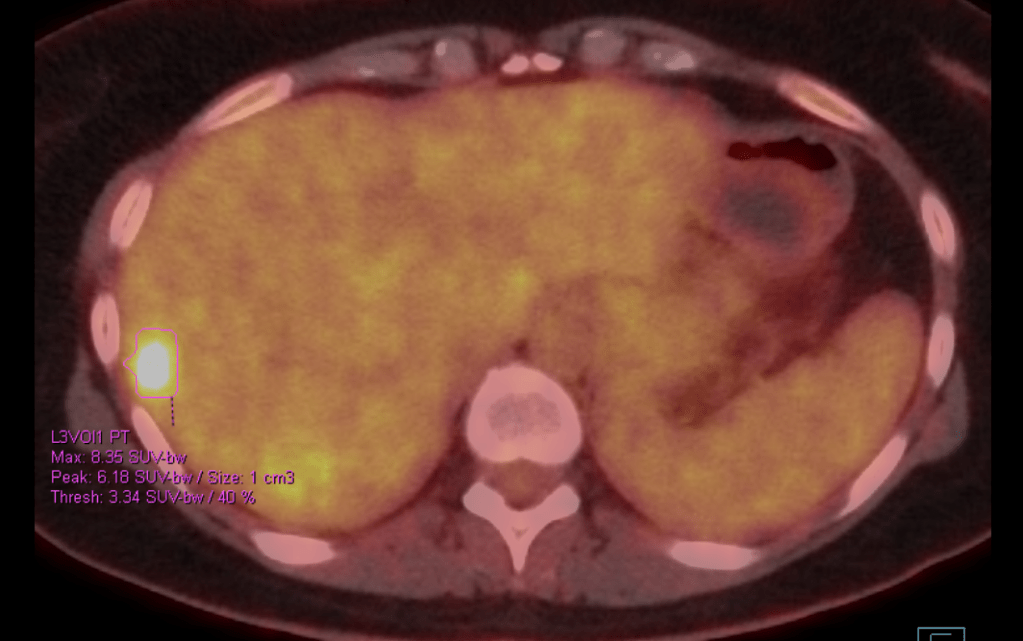
For day 2 of my visit, I had an early CT scan. Time to see more efficiency in action! Up until now CT scans haven’t shown my liver metastases very well. But the oncologist had assured me they do CTs differently at Big Cancer Center. In the past, most of my CTs have been performed with contrast only injected into me via IV. I’ve also had a couple of scans while in the hospital where I had to drink two bottles of contrast fluid. However, Big Cancer Center uses triple contrast. This final contrast would be rectal (i.e. up the bum). To me this seems like a lot of poison to take in, but the doctor assured me that in my case it was worth it.
The Prep
I reviewed the instructions multiple times on Monday to plan out how to comply.
First, I made sure to get up at 5 a.m. to eat a light breakfast while eating was still allowed. Then at 5:20am I started on my first bottle of water. Instructions were to chug two bottles (1000 mL) two hours before check-in. Gatorade was also in the acceptable beverages list, so I had a bottle of that on hand as well to sip for extra sustenance until my appointment.
I re-checked the instructions online and found there was yet another form added overnight. Got that taken care of online so I wouldn’t have to do it when I got there.
I arrived within two minutes of my scheduled time of 7:20am so I wouldn’t have to sit around waiting. They gave me a new hospital wristband for the day and, a short time later, a giant cup of the oral contrast. “Would you like water, Sprite, or Crystal Light?” I of course went with room-temperature water. I’d probably feel sick if I drank a jug full of Sprite, and Crystal Light wouldn’t be much better. I’m lucky, though. Some people are really sensitive to the taste of the contrast itself. I’m fine as long as they don’t decide to add any cilantro.
While sipping my drink, I tried to distract myself by looking around the room at posters for washing hands and recommending downloading an app to be able to find where you’re going in the hospital. I discovered right behind me a big board with people’s initials and the time they were scheduled to go into the CT. This is how I discovered that the total process time of 1-2 hours which was mentioned in the instructions was a lie. 9:20 a.m. meant two hours before I would even go into the machine. I kept sipping.
Fortunately, someone came in to sit down beside me and was willing to chat a bit. He had colon cancer, which is also a candidate for triple contrast (anything in the pelvic region), so I asked about it. He warned that it feels cold when it goes in. Good to know.
I had finished my drink. My butt was getting really tired of sitting there. And of course, my special type of scanxiety is the kind that eases up when I’m through with the scan. So it was a huge relief when I was finally called back. They had pants and shirts to change into and those horrible socks that are awkward to walk in. (This set of socks was about the right size for my feet, but they stuck to the floor a bit.) The pants were too long and had to be tucked into my socks, making me look like a goofball. But that’s easy enough.
Next up was getting the IV. I recently asked a nurse, “Are there people who never have problems getting an IV?” Apparently there are many. But not me and not today. “There appears to be a valve there. We’ll have to try somewhere else.” and “Sorry to tell you this, but this one isn’t going to work either.” I was walked down a super long hallway to another area where someone else successfully got the IV in. Just in time for my 9:20 scan time.
The Scan
They must have been behind schedule because I had to wait a bit more before I was finally taken back. I climbed onto the scanning bed and pulled down my pants enough for the tiny tube to be inserted into my rectum. Fortunately not at all as awkward as I anticipated, and I was ready when I felt the cold liquid inside me. After I laid on my back for a bit, I had this strange sensation like tiny bubbles rising up towards my belly button. Surely that meant it had infiltrated my innards as needed.
The CT machine whirled around me and the table slid in and out a couple of times before the IV contrast was injected into me. I hate the feeling of this poison running through my veins. It always makes me feel slightly nauseated and warm. And of course there’s that feeling like you’re peeing. This time it was even warmer than usual. Or hot, really. “The sensation will go away in a moment”, I repeated in my head trying to calm my nerves.
As the scanning bed went through that time, I felt a slight tickle in my throat just as I was prompted to hold my breath. Let me tell you, holding your breath when you’re fighting an urge to cough isn’t easy. It just made the urge grow. Finally, the machine said “Breathe normally” and allowed the opportunity for a tepid cough. The technician came in to check on me and agreed to bring me some water, though I wasn’t allowed to move my lower body still.
The CT machine started whirring more loudly again, and I laid back down eager to be done with whatever was still needed. This truly was nothing like the super quick CT scans I was used to. “They had better get some really good pictures from this,” was all I could think.
Recovery
Apparently, if you cough, it’s an indication that you are unable to walk. The tech escorted me down the hall with his hand on my back. Then someone else took over and grasped me by the arm. I hobbled around awkwardly in the sticky socks, resisting the urge to push these touchy people away from me.
Multiple people asked me about the tickle in my throat and the urge to cough. Apparently, this can be a reaction to the IV contrast. Was I having trouble breathing? Did my throat feel tight? etc, etc.
Eventually they left me alone on a chair between some curtains, saying that I could leave in 15 minutes. I finished the bottle of water and was starting to get cold but wasn’t sure if I was allowed to go over to the desk to ask for anything. I just waited. At some point the nurse came over to check again that I wasn’t actually dying. I wasn’t. I was cleared to change into my clothes and go home.
Once again I was escorted down the hallway. When I was directed to exit into the imaging center lobby, I pointed out that my IV hadn’t been removed yet. I probably should have guessed that the IV needed to be taken out in that curtained area, but my confidence had been wiped out. Anyhow, I was taken back over, got the IV out, and was finally headed back to the hotel a little over three hours after my appointment start time. Too late to satisfy my plan to grab a hot breakfast at the hospital cafeteria. Good thing I had plenty of snacks at the hotel.
Patient Portal
Back at the hotel, I checked the patient portal repeatedly to see if my scan results would show up. After seeing how quickly the blood test results came back, I was happily looking forward to getting my CT scan results in record time.
I’m not so stupid as to just keep checking forever, though. A web search found the information that CT results don’t show up until two days after the report is finalized. That’s better than the three day wait at my usual place, but still, Ugh.
Good thing I checked the portal, though. I found a visit summary that included:
“Patient expressed understanding that if she continues to have reactions from IV contrast that she will need premedication prior to her scans. She acknowledged understanding and was in agreement with this plan. All questions were answered.”
Wow. It’s a good thing I read that. I was wondering if they did consider it a reaction or not. Now I know that they already told me about it when I wasn’t listening, and I agreed to a plan to it when I wasn’t speaking. This is not something new. I’ve frequently seen lies inserted into charts so they can be used as “proof ” to cover their asses. But somehow I expected more from Big Cancer Center.
Well, all to do now is to wait and see if the results make it all worth while.